



Department: Gastroenterology
Estimated Cost : $3,000 - $20,000
Pancreatitis refers to the inflammation of the pancreas, an essential organ in the body responsible for producing digestive enzymes and insulin. When the pancreas becomes inflamed, it disrupts the normal digestive process and can lead to severe complications, affecting the overall health of the patient. The condition can either be acute (sudden onset) or chronic (long-term inflammation). Proper pancreatitis treatment is essential to prevent complications like tissue damage, diabetes, and even pancreatic cancer.
Understanding the different treatment options for pancreatitis and how to manage this condition is crucial for ensuring better health outcomes. In this guide, we will explore the causes, symptoms, and available treatment options for both acute and chronic pancreatitis, highlighting the importance of timely medical intervention.
Pancreatitis can manifest in two primary forms:
1. Acute Pancreatitis
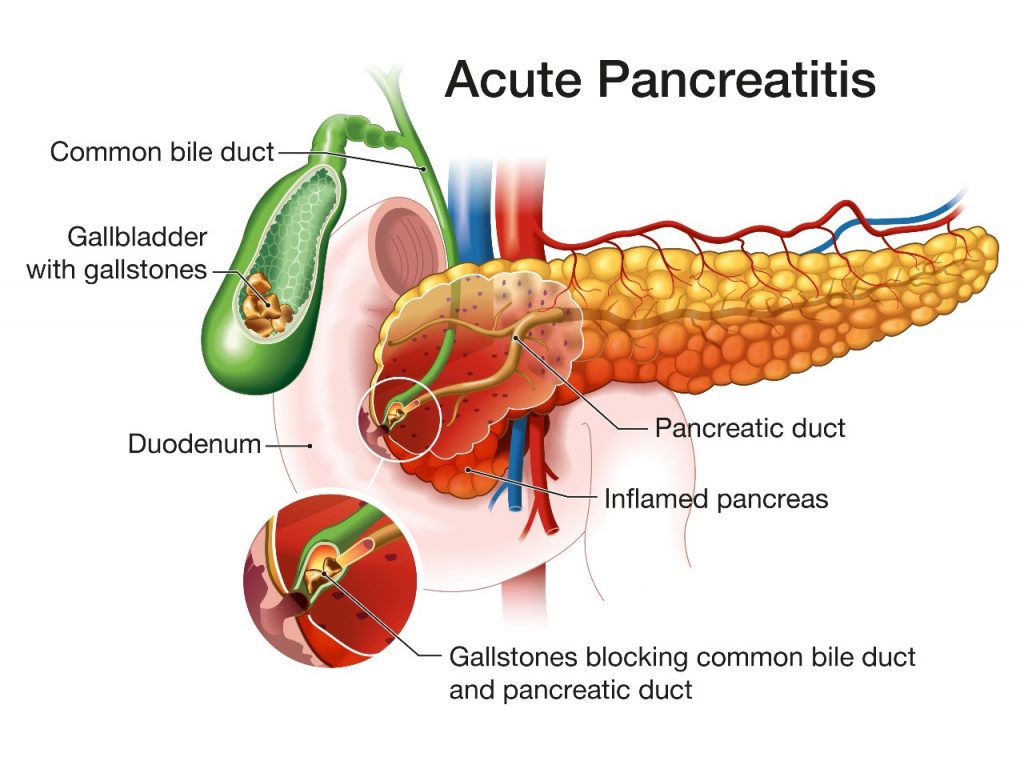
Acute pancreatitis is the sudden inflammation of the pancreas that can develop rapidly, causing significant discomfort and potential life-threatening complications. In most cases, acute pancreatitis is triggered by factors such as alcohol abuse, gallstones, medications, or viral infections.
Symptoms of Acute Pancreatitis:
Acute pancreatitis can range from mild to severe, with the potential to cause complications such as pancreatic necrosis, infection, or organ failure.
Treatment for Acute Pancreatitis: Treatment for acute pancreatitis typically begins with hospitalization. Resting the pancreas is essential, and patients are usually advised to refrain from eating solid food for a few days. Instead, intravenous fluids are administered to prevent dehydration and manage pain. The main goal of treatment is to control inflammation and relieve pain, allowing the pancreas time to heal.
In some cases, if acute pancreatitis is caused by gallstones, surgery may be required to remove the stones. Additionally, antibiotics may be prescribed if there is an infection, and certain medications may be used to manage pain. Depending on the severity of the condition, patients may need more invasive treatments, such as endoscopic procedures, to clear blockages or drains in the pancreas.
2. Chronic Pancreatitis
Chronic pancreatitis is a long-term inflammation of the pancreas that occurs when the organ is repeatedly damaged over time. This persistent inflammation leads to scarring and permanent damage, affecting the pancreas' ability to produce enzymes and insulin. Chronic pancreatitis is commonly caused by long-term alcohol consumption, but it can also result from hereditary factors, certain genetic conditions, and repeated episodes of acute pancreatitis.
Symptoms of Chronic Pancreatitis:
Treatment for Chronic Pancreatitis:
Chronic pancreatitis requires ongoing management. The treatment is focused on controlling pain, managing symptoms, and addressing complications. Medications such as pain relievers or opioid medications are often prescribed to alleviate pain. Enzyme replacement therapy is commonly used to help patients digest food, as chronic pancreatitis often leads to a deficiency in pancreatic enzymes.
If chronic pancreatitis is complicated by the development of pancreatic duct obstructions or cysts, an endoscopic procedure may be required to clear the blockage. For those with significant pancreatic damage, surgical interventions may be necessary to remove parts of the pancreas or drain fluid collections.
Managing lifestyle factors, such as avoiding alcohol and maintaining a low-fat diet, is crucial in preventing further damage to the pancreas. Patients with chronic pancreatitis may also develop diabetes over time, which will require insulin therapy to manage blood sugar levels effectively.
There are several treatment options for pancreatitis, which vary depending on whether the condition is acute or chronic. The goal is to address the underlying causes, relieve symptoms, and prevent further damage to the pancreas.
1. Hospitalization for Acute Pancreatitis
For most patients with acute pancreatitis, hospitalization is required to monitor vital signs, manage pain, and provide supportive care. Hospitalization often involves the following:
2. Surgical Intervention
If acute pancreatitis is caused by gallstones or other obstructions in the pancreatic duct, surgery may be necessary to remove these blockages. Additionally, for chronic pancreatitis, surgery may be required if there are severe complications like cysts or persistent pain that doesn’t respond to other treatments.
3. Endoscopic Procedures
In both acute and chronic pancreatitis, endoscopic procedures may be employed to drain fluid collections, remove blockages, or treat complications like pancreatic pseudocysts. These minimally invasive procedures are performed using a flexible tube with a camera, which allows the doctor to visualize and treat the affected areas without the need for large incisions.
4. Enzyme Replacement Therapy
For patients with chronic pancreatitis, enzyme replacement therapy is critical to manage malabsorption. Since the pancreas no longer produces enough enzymes, this therapy helps break down food and absorb nutrients, alleviating symptoms like diarrhea and weight loss.
5. Lifestyle Modifications
Dietary changes and lifestyle management are vital components of treating pancreatitis. Patients are encouraged to:
When it comes to pancreatitis treatment, choosing the right healthcare provider is crucial. Healtour Solutions offers patients access to top-tier healthcare facilities and specialists in India, ensuring high-quality and affordable care.
Why choose Healtour Solutions?
If you or a loved one are suffering from pancreatitis, don't wait. Get in touch with Healtour Solutions today to access expert care at affordable prices. Our team of specialists is ready to help you navigate your treatment journey and ensure a better quality of life. Contact us for a personalized consultation!
@2025 Healtour Solutions Pvt Ltd. All Rights Reserved.