Hysteroscopy
Department: Gynaecology
Estimated Cost : $500 - $1000
Discover the Precision of Diagnostic Hysteroscopy
What is Diagnostic Hysteroscopy
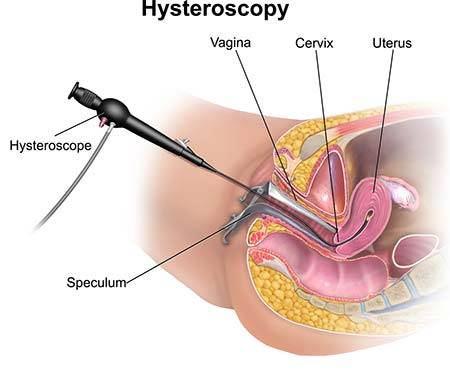
Diagnostic hysteroscopy is a minimally invasive procedure used to examine the inside of the uterus for diagnostic purposes. It involves the use of a thin, lighted tube called a hysteroscope, which is inserted through the vagina and cervix to provide a clear view of the uterine cavity.
This procedure is highly effective in identifying uterine abnormalities such as polyps, fibroids, adhesions, or unexplained bleeding. It is often recommended when less invasive diagnostic methods, like ultrasounds, do not provide sufficient clarity.
Diagnostic hysteroscopy is a critical tool in women’s healthcare, allowing doctors to make accurate diagnoses and plan effective treatments with minimal discomfort for the patient.
Who Needs Diagnostic Hysteroscopy?
Diagnostic hysteroscopy is recommended for individuals experiencing specific gynecological symptoms or conditions that require a closer examination of the uterus. Here are common scenarios where this procedure may be necessary:
- Unexplained Abnormal Uterine Bleeding: Helps investigate irregular periods, heavy bleeding, or bleeding after menopause.
- Infertility or Recurrent Miscarriages: Identifies structural issues in the uterus that may impact conception or pregnancy.
- Suspected Uterine Abnormalities: Diagnoses polyps, fibroids, adhesions, or uterine septum.
- Persistent Pelvic Pain: Evaluates uterine health to rule out internal issues causing discomfort.
- Post-Menopausal Bleeding: Helps determine the cause of bleeding and assess endometrial health.
- Abnormal Findings in Imaging Tests: Provides detailed insights when an ultrasound or MRI indicates abnormalities.
By offering a precise diagnosis, hysteroscopy ensures that treatment plans are tailored effectively to address the root cause of the issue.
The Diagnostic Hysteroscopy Process
Diagnostic hysteroscopy is a minimally invasive outpatient procedure. Here's what you can expect during the process:
- Preparation:
- Your doctor may recommend scheduling the procedure soon after your menstrual cycle for optimal visibility of the uterine cavity.
- You might be advised to avoid heavy meals and take prescribed medications beforehand.
- Procedure:
- Local or General Anesthesia: Depending on the complexity, local anesthesia or sedation may be used for comfort.
- Insertion of Hysteroscope: A thin, lighted tube (hysteroscope) is inserted through the cervix into the uterus.
- Visual Examination: The doctor examines the uterine lining using a small camera attached to the hysteroscope. Saline or gas may be introduced for better visibility.
- Duration:
- Typically takes 10–30 minutes, depending on the findings.
- Recovery:
- Most patients resume normal activities within a day. Mild cramping or spotting may occur for a few days.
Diagnostic hysteroscopy offers a detailed view of the uterine cavity, making it invaluable for accurate diagnosis and treatment planning.
Benefits of Diagnostic Hysteroscopy
Diagnostic hysteroscopy offers numerous advantages, making it a preferred method for evaluating uterine conditions:
- Enhanced Accuracy:
- Provides a direct view of the uterine cavity, ensuring precise diagnosis of abnormalities like fibroids, polyps, or scar tissue.
- Minimally Invasive:
- Eliminates the need for major surgery, resulting in minimal discomfort and quicker recovery.
- Outpatient Procedure:
- Often performed on an outpatient basis, allowing you to return home the same day.
- Dual Purpose:
- Can transition into a therapeutic procedure if minor issues are detected, such as removing polyps or fibroids.
- Improves Fertility Assessment:
- Helps identify and address uterine issues that may be affecting fertility.
- Quick Recovery:
- Most patients resume daily activities within 24 hours with minimal side effects.
Diagnostic hysteroscopy combines efficiency, precision, and patient comfort, making it an invaluable tool in gynecological care.
Indications for Diagnostic Hysteroscopy
Diagnostic hysteroscopy is recommended for various gynecological conditions and concerns, including:
- Abnormal Uterine Bleeding:
- To investigate heavy, irregular, or postmenopausal bleeding.
- Infertility or Recurrent Miscarriages:
- Helps evaluate structural abnormalities or other uterine issues impacting fertility.
- Suspected Uterine Fibroids or Polyps:
- Provides a clear view to confirm and locate these growths.
- Endometrial Thickening:
- Assesses conditions like hyperplasia or other uterine lining irregularities.
- Retained Products of Conception:
- Ensures the uterus is free from tissue after a miscarriage or delivery.
- Congenital Uterine Abnormalities:
- Diagnoses malformations like a septate or bicornuate uterus.
- Foreign Bodies:
- Detects and removes items like intrauterine devices (IUDs) embedded in the uterine wall.
- Pre-IVF Uterine Evaluation:
- Ensures the uterine environment is optimal for embryo transfer.
Diagnostic hysteroscopy is a versatile tool, addressing both diagnostic and preliminary therapeutic needs for a wide range of gynecological issues.
Risks and Limitations of Diagnostic Hysteroscopy
While Diagnostic Hysteroscopy is a safe and widely-used procedure, it’s essential to understand the potential risks and limitations:
Risks
- Mild Discomfort: Patients may experience slight cramping or spotting post-procedure, which typically subsides within a day or two.
- Infection: Rare but possible, especially if proper post-procedure care isn’t followed.
- Allergic Reactions: Some individuals may react to the anesthesia or fluids used during the procedure.
- Uterine Perforation: Extremely rare, occurring in less than 1% of cases, and is more common in individuals with complex uterine conditions.
Limitations
- Not Therapeutic in All Cases: While minor abnormalities can be treated during the procedure, significant surgical interventions may require a follow-up hysteroscopy or alternative procedures.
- Access Restrictions: Patients with severe uterine scarring or a narrow cervix may face challenges during the procedure.
- Fertility Outcomes: While diagnostic hysteroscopy identifies issues, resolving them may not guarantee improved fertility outcomes in all cases.
Why Choose Healtour Solutions for Diagnostic Hysteroscopy
At Healtour Solutions, we provide a seamless and hassle-free experience for patients seeking Diagnostic Hysteroscopy. Here's why you should choose us:
- Expert Medical Network: We partner with top fertility centers and hospitals in India, ensuring you receive the best care from experienced specialists.
- Personalized Care: We understand that every patient’s needs are unique. Our team works closely with you to provide customized treatment plans that align with your health and personal goals.
- Comprehensive Services: From initial consultation to post-procedure follow-up, we offer a full range of services, ensuring you have all the support you need throughout your treatment journey.
- Cost-Effective Solutions: We offer affordable treatment options without compromising on quality. Our transparent pricing ensures you get the best value for your money.
- Seamless Travel Assistance: For international patients, we provide end-to-end travel assistance, including flight bookings, visa arrangements, and accommodations, ensuring a smooth medical tourism experience.
- Trusted by Patients Worldwide: Our satisfied patients come from all over the world, and their trust in our services is a testament to the high standards we uphold.
FAQ’s
1. What is diagnostic hysteroscopy?
Diagnostic hysteroscopy is a procedure used to examine the inside of the uterus using a thin, flexible tube. It helps diagnose conditions like fibroids, polyps, or uterine abnormalities.
2. How long does the diagnostic hysteroscopy procedure take?
The procedure typically takes around 20 to 30 minutes. It is minimally invasive and often performed on an outpatient basis.
3. Is diagnostic hysteroscopy painful?
While it may cause mild discomfort or cramping, most patients experience only minimal pain. Local anesthesia or sedation is used for comfort.
4. How soon can I resume normal activities after the procedure?
Most women can resume normal activities within a day or two. However, it’s advised to avoid heavy lifting or strenuous exercise for a short period.
5. Is diagnostic hysteroscopy safe?
Yes, diagnostic hysteroscopy is generally a safe procedure. Risks are minimal but may include infection or bleeding, which are rare.
6. Can diagnostic hysteroscopy treat conditions?
While diagnostic hysteroscopy is mainly for examination, it can also treat minor conditions, such as removing polyps or fibroids, during the procedure.
7. Do I need to fast before the procedure?
Usually, fasting is not required for diagnostic hysteroscopy unless general anesthesia is used. Your doctor will give specific instructions before the procedure.
8. What is the recovery time for diagnostic hysteroscopy?
Recovery is quick, with most patients experiencing only mild discomfort and a small amount of spotting. Full recovery typically happens within a few days.
9. Can diagnostic hysteroscopy be performed during menstruation?
It is not usually recommended to perform the procedure during menstruation as it can interfere with visibility. Scheduling it during a different time of the cycle is preferred.
10. What should I expect after the procedure?
Post-procedure, mild cramping and spotting are common. If you experience heavy bleeding or fever, contact your doctor immediately for advice.
 Get an Opinion
Get an Opinion
